IN THIS LESSON
Staying Well:
HIV/STI Testing & Prevention
Learning about HIV and STI prevention does not mean you did anything wrong. It means you are taking care of yourself. Whether this is information you wish you had years ago or something you are just starting to explore, it belongs to you. Take what is useful, come back when you need it, and remember that staying well is a form of power.
Staying well is about more than avoiding harm. For Black LGBTQ+ youth, wellness is also about access, dignity, and having information that actually speaks to our lives. Too often, conversations about HIV and STIs show up wrapped in fear, silence, or judgment. They focus on what not to do instead of what helps us stay healthy, connected, and in control of our bodies. At TKO, we believe that prevention should feel empowering, not shaming. Knowing your options is one way we keep us safe.
HIV and other sexually transmitted infections are part of the real world, not a personal failure or a moral issue. They affect people across genders, sexualities, and communities. What makes Black LGBTQ+ youth more vulnerable is not who we are, but the barriers we face. These include stigma, medical racism, transphobia, lack of affirming care, and misinformation that spreads when accurate resources are hard to find. Naming those barriers matters, because it reminds us that needing information or support does not mean you did something wrong.
Prevention is not one-size-fits-all. For some people, it looks like regular testing. For others, it looks like condoms, PrEP, PEP, treatment, honest conversations with partners, or harm reduction strategies that meet them where they are. Many people use more than one tool, and some choose different options at different points in their lives. All of these choices are valid. The goal is not perfection. The goal is having enough knowledge to make decisions that feel right for you.
Getting tested is a form of care, not an admission of guilt. Knowing your status can bring peace of mind, open doors to treatment if needed, and help you protect yourself and others. People living with HIV can and do live long, full lives, especially with access to care. Treatment works, and when someone’s viral load is undetectable, HIV cannot be passed on through sex. That is not just science. It is liberation from fear and stigma.
We also know that navigating healthcare, especially in Alabama, can feel overwhelming. You may worry about confidentiality, cost, or whether a provider will respect your identity. Those concerns are real. You deserve care that affirms who you are and keeps your information private. You have the right to ask questions, to advocate for yourself, and to walk away from providers who do not treat you with respect. Support exists, even when the system feels stacked against you.
At its core, HIV and STI prevention is about staying well enough to live your life fully. It is about pleasure, safety, boundaries, and care for yourself and your community. You deserve information that is honest, stigma-free, and rooted in respect. This resource is here to offer tools, not rules. Take what you need, come back when you are ready, and remember that you are not alone. We keep us safe.
We keep us safe.
〰️
We keep us safe. 〰️
Frequently Asked Questions
This FAQ brings together questions we hear all the time from Black LGBTQ+ youth. These are the questions people often wish they had answers to before becoming intimate, after a scare, or while trying to take better care of themselves.
So much information can be overwhelming, but you do not need to read this from top to bottom. Jump to what you need, take your time, and know that no question here is silly, wrong, or shameful.
Frequently Asked Questions
This FAQ brings together questions we hear all the time from Black LGBTQ+ youth. These are the questions people often wish they had answers to before becoming intimate, after a scare, or while trying to take better care of themselves.
So much information can be overwhelming, but you do not need to read this from top to bottom. Jump to what you need, take your time, and know that no question here is silly, wrong, or shameful.
Testing: What People Wish They Knew Beforehand
-
HIV is a virus that affects the immune system. With modern treatment, it can be managed as a chronic condition.
-
There is no cure yet, but treatment is highly effective. People living with HIV who are on treatment can live long, healthy lives.
-
For many people, it looks like taking medication, going to regular medical appointments, and living full lives with relationships, goals, and joy.
-
Yes. HIV does not prevent someone from having intimacy, love, or connection.
-
Undetectable means the amount of HIV in someone’s body is so low that it cannot be measured by standard tests. When someone is undetectable, HIV cannot be passed on through sex.
-
No. This is known as undetectable equals untransmittable (U=U).
-
With treatment, HIV can be managed similarly to other long-term conditions. Stigma often causes more harm than the virus itself.
Communication, Consent & Boundaries
-
Awkward does not mean wrong. These conversations are part of care. You do not need perfect words.
-
That can be a sign to pause and think about what you need to feel safe. You deserve mutual respect.
-
You are not required to share everything. What matters is honesty about things that affect consent and safety.
-
You can ask directly and respectfully. Their response can help you decide what feels right for you.
-
Pressure is not consent. You have the right to say no or to slow things down.
-
Yes. Always.
Shame, Timing &
Self-Compassion
-
No. There is no deadline for taking care of yourself.
-
That is not your fault. Information is often withheld or stigmatized.
-
You deserve support. Testing, talking to someone you trust, or reaching out to a provider can help.
-
No. Learning is growth, not failure.
-
Be patient with yourself. Curiosity and care are signs of strength.
Want to learn more or go deeper?
Here are a few resources to check out:
For clear, up-to-date information on HIV, testing, and treatment, LEARN MORE HERE. (National Institutes for Health)
For accessible sexual health education and testing information, LEARN MORE HERE. (National HIV Alliance)
For the basics about HIV and STIs, including prevention tools LEARN MORE HERE. (Planned Parenthood)
For LGBTQ+-affirming health information and resources, LEARN MORE HERE. (Scarleteen)
-
Yes. Many HIV and STI infections do not cause symptoms right away, or at all. Feeling fine does not always mean everything is fine. Testing gives you information, not a diagnosis you didn’t ask for. It is one way to stay informed about your health.
-
Some people choose to get tested before having sex with a new partner. Others test regularly as part of routine care. There is no single right timeline. What matters is choosing a plan that feels realistic and supportive for you.
-
Different infections have different window periods, which means they show up on tests at different times. A provider or testing site can help you figure out when to test and whether follow-up testing makes sense. Getting tested sooner is still better than waiting indefinitely.
-
Many sexually active people test every three to six months, while others test yearly or when partners change. There is no rule that applies to everyone. Testing frequency can change over time.
-
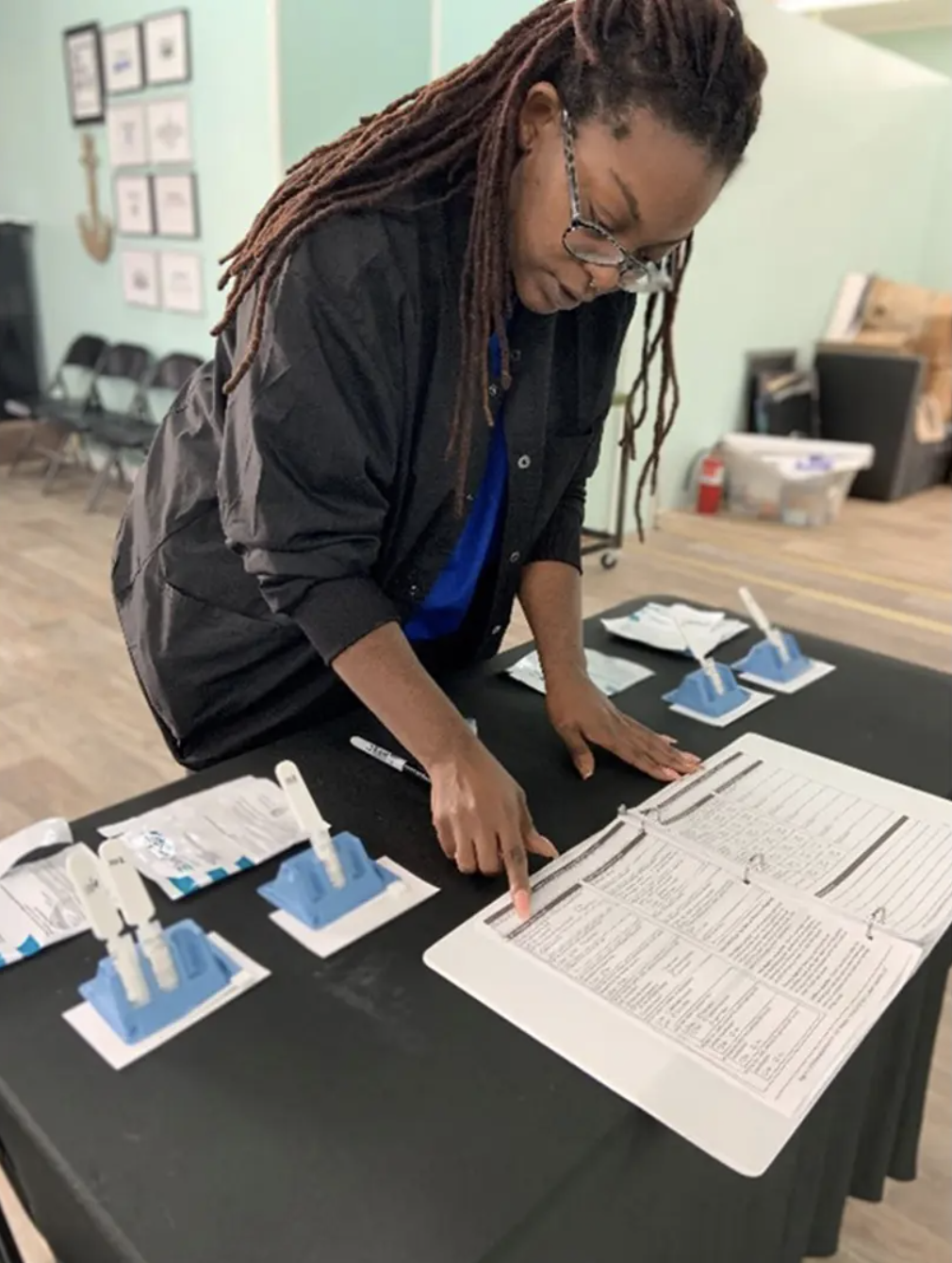
Testing is usually quick and straightforward. It might involve a finger prick, blood draw, swab, or urine sample. Providers should explain what they are doing and answer your questions. You have the right to understand what is happening to your body.
-
Yes. Some people find it helpful or reassuring to test together. This can be part of building trust and shared care, but it is always optional.
-
In many cases, yes. Laws vary by location, but many clinics offer confidential testing for minors. You can ask about confidentiality before testing so you know what to expect.
-
No. Testing means you care about your health. That is it.
Prevention Tools:
Knowing Your Options
-
Options include condoms and barriers, regular testing, PrEP, PEP, and HIV treatment. Many people use more than one tool.
-
Condoms greatly reduce the risk of many STIs and HIV, but they do not protect against everything. They are still an important and effective option.
-
PrEP (Pre-Exposure Prophylaxis) is a medication taken by people who are HIV negative to prevent HIV. It can be a good option for people who want additional protection.
-
PEP (Post-Exposure Prophylaxis) is a short-term medication taken after a possible HIV exposure. It must be started quickly, usually within 72 hours.
-
Some people experience mild side effects, especially at first. A provider can help you weigh benefits and concerns.
-
Some people do, some do not. Prevention can be layered or simple depending on your needs.
-
Yes. Your choices can change as your relationships, health, or circumstances change.
Assessing Support & Care
in Alabama
-
Testing is available at clinics, community health centers, and some local organizations. TKO can help connect you to affirming options.
-
Many testing sites offer free or low-cost services. You can ask about cost before your visit.
-
Community organizations, online directories, and word of mouth can help identify affirming care. You can visit the TKO resources sheet here.
-
You deserve respectful care. You can correct them, ask for another provider, or leave if you feel unsafe.
-
Healthcare providers are required to protect your privacy. You can always ask about confidentiality.
-
Organizations like TKO exist to help you access information, resources, and support.